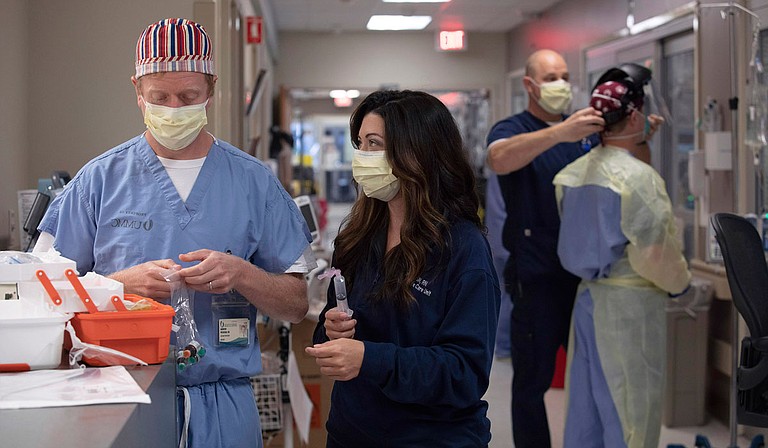
Dr. Andy Wilhelm and RN Ashley Moore’s medical intensive-care unit is strained to capacity with coronavirus patients. Photo courtesy UMMC Communications
Wednesday, July 22, 2020
Ashley Moore is saying goodbye. She does not offer a traditional farewell, neither the last rites of a priest nor the comforting touch of family. "I'm gonna stay here with you the whole time to support you. I'm gonna make sure you're comfortable," she says to a breathless COVID-19 patient.
She places the ventilator on her patient, soothing the best that she can, treating the myriad complications of an organ system in terminal decline—but for many, little she can do helps, and nothing works.
"Hours later, days later, a week later ... they pass away," Moore says in a later interview. The isolation, more than anything else, haunts her. "They didn't get to talk to their children before they passed, or their loved ones. You are the last person they talked to."
She said goodbye to a victim of coronavirus once again only days before her interview. For her, it was the 11th time. For Mississippi, it was one of more than a thousand lonely deaths just like it.
Moore is nurse manager at the Medical Intensive Care Unit of the University of Mississippi Medical Center, a unit entirely devoted to severely ill coronavirus patients. She spoke to the Jackson Free Press alongside Dr. Andy Wilhelm, medical director for the same unit.
Both talked candidly about their fatigue and their resolve, and the urgency needed from all Mississippians as the virus rampages through the hospital system, leaving UMMC and many other hospitals across the state packed full of critically sick and dying patients.
"The hardest part for us is knowing that we're operating at full capacity. And we know that there are a lot more people that are going to need critical care services over the next few weeks to months. We're already going full speed. But we're going to have to run faster," Wilhelm said.
'Exceptionally Sick'
For many Mississippians, coronavirus metrics are numbers on a screen. Plateaus become spikes, triple digits become quadruples. All-important data reduce the human catastrophe of the virus to a daily drip of vaguely threatening news. For Moore, Wilhelm and the many other health-care workers who spoke to the Jackson Free Press, it is the cadence of their lives, the increasingly rapid drumbeat forcing the countless decisions they make in any given day.
"It's more hours of work. It's less time for patients. It's less time talking with families. It's knowing that when you spend less time with the person that you may not be taking as good care of them as you would've otherwise," Wilhelm said.
"Nursing is all about time management," said nurse Alex Marten, a pseudonym, whose ICU at a different Mississippi hospital is more than half COVID-19 patients. "It doesn't necessarily require a lot of strength, or dexterity, but you have to manage 20 to 30 tasks at a time, all day. It's like spinning plates." And even the smallest mistake could cost a patient dearly, or expose the caregiver to the disease itself.
"These people are critically ill. Coronavirus patients are exceedingly complicated and exceptionally sick," Wilhelm said. "More sick than the typical non-coronavirus patients."
"And with them, the details matter," Moore added.
Details, endless details, emerging from the grinding torture to which the coronavirus exposes the human body. To call it a respiratory disease is darkly comic in light of the litany of damages Wilhelm lists: renal failure, strokes, clots, muscular degeneration, a vast and deadly constellation of cardiac diseases. All require precise and dedicated care beyond the consistent respiratory symptoms, which are horribly lethal on their own.
Moore and Wilhelm's unit serves coronavirus disease patients without coronavirus itself. The virus has already torn its way through their system, leaving them free of the cause and suffering from the symptoms. "Once the virus is gone, they're left on dialysis—or they're left on the ventilator because their lungs are too scarred to breathe adequately anymore," Wilhelm said.
That lingering damage is just another reason the rapid spread of the virus so threatens the state's health-care system. Wilhelm describes the cyclical nature of treatment and recovering.
"You're having the same conversation over and over again with patients: We don't know if you're going to live or not. 'Am I getting better?' Not really. Or maybe a little bit. Or you're still the same, three weeks in. ... When you have to have that conversation every day...," Wilhelm pauses, searching for the words. "It's difficult."
'Please Don't Make This Worse'
Below the Medical Intensive Care Unit lies the Emergency Department, the point of first contact for most patients who arrive at UMMC. There, RN Catie Carrigan and Dr. Risa Moriarity, executive vice chair of Emergency Medicine, attempt to stabilize everyone from trauma victims to a rising tide of the critically ill and coronavirus-afflicted.
"Working in the ER, we're prepared for anything that comes through the door. We take care of the sickest people in Mississippi," Carrigan said in an interview with the Jackson Free Press. "That being said, I don't think anybody could have prepared us for something of this velocity."
The hospitalization numbers for COVID-19 lag behind new infections, but late June and July's unprecedented spike has UMMC well beyond its capacity. It is the nightmare scenario that State Health Officer Dr. Thomas Dobbs predicted in grim detail only weeks before.
Back in March, immediately following the arrival of coronavirus in Mississippi, with the eyes of the nation fixed on the horror in New York, Carrigan and Moriarity braced for the worst.
"We had that feeling of the calm before the storm," Moriarity said. But the surge didn't come, not then. May brought an influx of COVID patients and those who had been delaying medical care, but the increase was manageable—for a while.
"Over the past two weeks, things here have become...," Moriarity halts. "Very, very challenging." Like Wilhelm describing his MICU, the urgency of the moment and the need for poise and calm pull her words in different directions. "I won't say unmanageable, because we're still trying, but this is the worst it's ever been."
Describing the situation by the numbers is easier. "Our hospital is at capacity. We don't have ICU beds. We don't have (medical-surgical) beds. We are currently this morning boarding 35 people in the emergency department who need beds upstairs ... We're managing ICU patients down here in the ER. We're managing other patients, some COVID, some not, but regardless, they don't have any beds.
"St. Dominic and Baptist are in similar situations. All the large hospitals in the state are at capacity," Moriarity says.
Carrigan is seeing things that should never happen in an emergency environment. "I had a trauma patient the other day that we kept in the ED for 36 hours," she said. "He was there when I arrived for my shift one day, and he was still there when I arrived for the next."
Both Carrigan and Moriarity have seen things that shatter the illusion that coronavirus is an affliction of the elderly or the already ill. For Moriarity, it was a patient in their early thirties, whose blood thickened and clotted, leaving their lungs riddled with pulmonary embolisms. For Carrigan, it is young, formerly healthy patients—the kind for whom the expected illness would be a week of dry coughing—sent up to intensive care for ventilation and a slim chance of survival.
"Young people feel a bit invincible," Moriarity laments. "COVID does not discriminate. It doesn't care who you are." And the onset of its most severe forms is terrifyingly quick: "You can be having a conversation one moment and on a ventilator the next."
For the two ED workers, the issue of prevention is painfully simple. At times they plead for assistance from the public. "All that we ask is that you wear masks, wash your hands and stay away from each other," Carrigan said. "I just don't think those are difficult steps to take ... but we get pushback all the time." At times, there is a barely concealed fury. "We see people out in public places without masks all the time," Moriarity added.
"I'm gonna be real honest with you," Carrigan cuts in. "It just makes me really angry."
Outside the walls of the ED, hoaxes swirl: laminated cards falsely inform store owners that the carrier is not legally obligated to wear a mask. Memes warn of bogus suffocation threats from masks that nurses and doctors regularly wear for days on end.
"Please don't make this worse for us," Moriarity said, suddenly sounding very tired. She repeats herself. "Please don't make this worse for us."
Minutes Lost, Lives Threatened
Across Mississippi, a flood of coronavirus is congesting ICUs and transfer routes alike. The Mississippi State Department of Health tracks the metrics daily: In July, months of cautious optimism dissipated in a matter of weeks. Data that previously depicted an uneasy and unending "plateau" now show horrifying upward trends in every category.
It started with syndromic surveillance: an unseasonable uptick in emergency-department visits for respiratory symptoms. Then, the case numbers spiked. The false security of the hot summer months and an end to most official quarantine procedures drew out public gatherings beyond all sense and safety, and the numbers soared.
During the period between July 15 and July 21, only a single day dipped below 1,000 plus new cases, culminating in a staggering 1,635 new reports just before press time. The hospitalizations derived from these unprecedented numbers are yet to come, a tidal wave that Dobbs warns may swallow the system whole.
Hospitalizations inevitably follow the soaring numbers, with Dobbs estimating 85 hospitalizations for every 500 cases, ICU admission and ventilator use rising along with it.
On July 18, MSDH released data charting the remaining hospital capacity across Mississippi's nine "health districts." District Five, which includes Hinds, Rankin and Madison County, as well as the state's largest hospitals and only level-one trauma center, shows the most distinct lack of capacity across Mississippi.
But statewide, intensive care units and medical-surgical units show a near doubling of their COVID-19 patients over the last month, a trend Dobbs assured the Jackson Free Press on July 20 would continue with the spiking numbers.
"Within two weeks or so, we anticipate that we'll exhaust our surge capacity," Dobbs said. "We may be at crisis standards of care in the next few weeks if we're not careful. If we don't see a decrease in transmission immediately, then it's pretty likely the health-care system is going to be overwhelmed."
At this stage, the strain of coronavirus thoroughly endangers all Mississippians. But the state's existing inequities—chiefly unequal access to health care, which Dobbs discussed at length in an earlier interview with the Jackson Free Press—are further stressors on the state's Black populations, which have remained disproportionately victimized by COVID-19 for the duration of the pandemic in Mississippi.
To understand the full impact of coronavirus' crushing weight requires looking beyond the upper-tier hospitals at the core of the system. Critical-access hospitals dot the lesser-populated regions of Mississippi like spokes on a wheel, many without active ICUs of their own. They depend on a rapid system of transfers for many of their sickest or most injured patients, a transit network in which lives can be saved or lost in minutes.
"You come in, you've had a wreck—you've got brain trauma. We're looking to fly you to UMMC because that's the level-one trauma center in the state. Well, what if we can't get you there because they're at surge capacity levels and cannot take another patient?" asked Lee McCall, CEO of Neshoba County General Hospital in Philadelphia.
"We start looking at different hospitals. It takes 20, 30, 40 minutes longer to get you somewhere. Delays of care cause bad outcomes. Every minute counts," McCall stressed. "That's the scenario everyone's dealing with."
McCall admitted to struggling with explaining the severity of the situation to the community at large. "People just don't understand it. They don't get it."
He recalled a particularly elusive patient, discharged after receiving a COVID-19 test. "We call them, let them know they're positive, that we had a hard time contacting them. 'Oh, well, I'm sorry. I'm out of town on vacation.' You're kidding me," he said.
The patient was not kidding.
At South Sunflower County Hospital in Indianola, Infection Control and Employee Health Nurse Henley Harrell acknowledged the gridlock in the transfer system has them sending some patients out of Mississippi entirely. "We've had to transfer some to ... Memphis and Little Rock. Bed availability has been difficult for COVID patients and others—trauma patients, things like that," she said.
The weight of the pandemic has taken a physical and psychological toll on the state's health-care providers. "We're from a small town. We're taking care of our own ... our friends and our family. It has been very emotional for the staff," Harrell said.
McCall had a laconic warning for the Mississippians still not taking the virus seriously: "Everything's fine. So long as you don't need the hospital."
'And Then You Lose Them'
Every doctor, nurse, technician and administrator interviewed for this story adamantly insisted on the basic principles of infection control that now underpin the state's coronavirus prevention strategy. Some raged, some wept. Most begged: Wear a mask. Stay distanced. Stay out of enclosed spaces. Stay out of large groups.
No region or county is spared the stress and suffering of coronavirus, from the orbit of Memphis to the center of the state, down to the Gulf Coast. Outside Mississippi, the situation looks equally grim: The out-of-state transfers that currently keep the most dire cases moving are not permanently guaranteed.
In Jackson, at Moore and Wilhelm's MICU, the onslaught is merciless. The ebb and flow of the virus have dictated their lives for weeks on end. So has the nation's mercurial approach to its containment and treatment.
"It's the most emotionally difficult thing I have taken care of as an intensive care unit physician," Wilhelm said. "You put a lot of physical and mental equity in these folks. ... You get to know them. You get to know their families—as best you can over the phone. And then you lose them."
Every new treatment, every twist in the world's understanding of the cruel virus at the source of the pandemic, leaves caregivers stricken with anxiety over past mistakes. "There's always this question in the back of your mind: Are we doing this right?" Wilhelm said.
"Then you come in the following day just to do it all over again," Moore added.
Wilhelm freely admits his sleep is fleeting and troubled. He tries desperately to quarantine himself from the barrage of news, repeating to him what he bears witness to on a daily basis. But there is little point in hiding. "It's everywhere," he said.
The images are constant, the work unrelenting. "We're putting somebody on the ventilator while they're crying at the same time—they're looking up at you with tears rolling down the side of their face. I'm pushing sedatives, putting them on life support," Wilhelm described.
"You throw everything at them, kitchen sink," Moore said.
And then they say goodbye.
State intern Julian Mills contributed to this report. Email state reporter Nick Judin at [email protected].



Comments
Use the comment form below to begin a discussion about this content.
Sign in to comment
Or login with:
OpenID